Cervical Myelopathy
Definition
Myelopathy is abnormal function of the spinal cord most often caused by pressure from disc bulges, bone spurs or spinal soft tissues. Patients with myelopathy have difficulties with hand function and poor balance.
Basic anatomy and causes of myelopathy
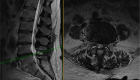
The spinal cord runs through the canal formed by bones in the neck (cervical spine), mid-back (thoracic spine) and upper part of the lower back (lumbar spine). Pressure on the spinal cord happens most often in the neck because it is the most mobile part of the spine.
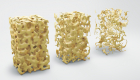
The spinal canal may narrow as a result of arthritis, trauma, disc bulges, bone spurs or thickening of the surrounding soft tissues causing pressure on the cord. Infection and tumors growing within the spinal canal may also cause myelopathy.
Because of pressure on the cord, internal inflammation and swelling develop. As the result, nerve signals do not travel easily through the cord from the arms and legs to the brain in either direction causing the symptoms of myelopathy.
Symptoms of myelopathy
The patient may experience a range of symptoms including clumsiness in the hands (difficulty handling small objects, like picking up coins, buttoning shirt) and worsening balance (called ataxia). Poor balance is mostly pronounced in the dark, when the person cannot control position of his/her body in space relying on vision.
In severe cases of myelopathy, patients may develop weakness in the arms and legs and even lose control of the bladder and bowel function.
Even though myelopathy by itself is a painless condition, pain may be present as a result of arthritis in the spine. Pinched nerves may also cause pain extending down the arms.
Diagnosis myelopathy and additional studies
Myelopathy may be suspected based on the history and physical examination, demonstrating abnormal hand function, poor balance and abnormal reflexes.
While these findings on physical examination may suggest myelopathy, the final diagnosis is made using modern imaging:
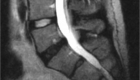
- MRI (Magnetic Resonance Imaging) is the most reliable diagnostic study for pressure on the spinal cord.
- CT (Computed Tomography) and X-rays allow a closer look at the spine deformities and bony structures. They are often used for surgical planning.
- Electrodiagnostic study (EMG) may be helpful in patients with arm pain.
Can other conditions present as myelopathy?
Symptoms similar to myelopathy may be caused by other conditions affecting the brain, spinal cord and nerves in the arms and legs. If some of the neurological findings do not exactly match findings on imaging, additional evaluation by a neurologist and advanced imaging like brain MRI may be required.
Treatment
Patients with severe or quickly progressing myelopathy typically require surgical decompression (removing pressure) of the spinal cord.
At the same time, patients with mild myelopathy may be closely monitored for a prolonged period. A short-term cervical collar, physical therapy for balance training and occupational therapy to improve hand function may be helpful.
If symptoms worsen, surgical decompression is the only treatment option to prevent further progression.
Stop letting spine pain control your life. Schedule your consultation with me today and take the first step towards lasting relief. Your journey to a pain-free life begins now. Click here to book your appointment.
What is the natural history of myelopathy? When is surgery recommended?
Symptoms of myelopathy tend to slowly worsen over time. In some patients the symptoms will remain stable or even improve over the years, while in others they may progress with different speed (up to 60% of patients after three years).
At this point we cannot reliably predict who will develop rapid progression and thus have to discuss treatment options separately with each patient. Recent studies suggest a more aggressive approach to treatment of myelopathy in cases with advanced or rapidly progressing symptoms.
What kinds of surgery are available to address myelopathy?
There are several options when it comes to surgery for myelopathy:
- Surgery done from the front of the neck:
- Anterior cervical discectomy and fusion (ACDF);
- Cervical corpectomy;
- Surgery done from the back of the neck:
- Laminectomy and posterior instrumented fusion;
- Laminoplasty (motion preserving procedure).
Decision to use one or the other procedure depends on several factors, including:
- Whether the pressure occurs from the front or back,
- Number of levels that need to be decompressed,
- If there is a neck deformity,
- Whether there is abnormal movement between the bones.
Is there a risk of paralysis if surgery not performed?
With significant narrowing of the spinal canal there is a small risk of injury to the spinal cord and weakness in the arms and legs. This may occur in cases of uncontrolled movement in the neck that may happen after a motor vehicle accident or a fall, etc.
This risk is very small and based on recent research by itself, is not considered an indication for prophylactic surgery.
Safety precautions if surgery is delayed.
Even though the risk of paralysis is very small, certain precautions are recommended:
- Always use the headrest in the car to prevent uncontrolled neck movement if your car is hit from behind;
- Take measures to prevent falls in your house: remove rugs, turn on the lights at night, use a walker if you feel unsteady;
- Avoid chiropractic manipulation of the neck.
If a non-spine surgery planned with general anesthesia, you should discuss it with your spine surgeon to decide if it is safe. The surgical team should take certain precautions since you cannot control position of your neck while under anesthesia.
If you like our materials, please subscribe to our newsletter to learn about spine conditions, new available treatments and how to keep your spine healthy.